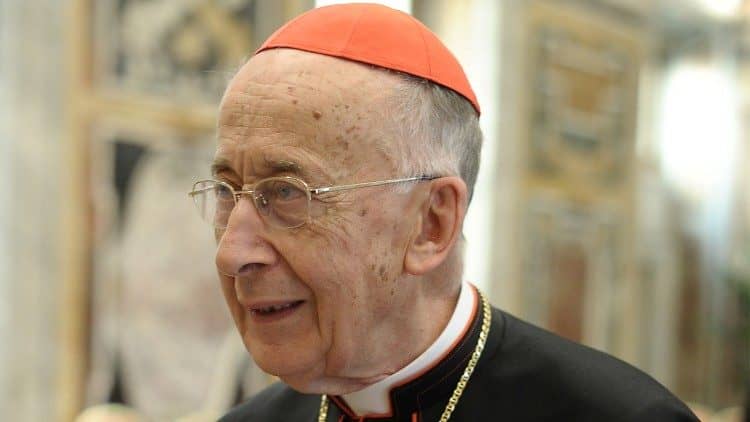
LEICESTER, United Kingdom – Bishop John Sherrington is the Lead Bishop for Life Issues in England and Wales.
As the United Kingdom’s Parliament fast approaches the final vote on a law for legalizing “assisted dying” – which critics points out is allowing doctors to help patients commit suicide, Sherrington called on the British people to contact their representatives in Parliament to oppose the Bill.
When the Bill was first voted on, it included a promise of several supposed “safeguards” – including limiting it for those suffering great pain and requiring a judge to approve it. However, most of these have been removed from the Bill as it reaches its final stage.
RELATED: As England leans closer to legalizing assisted dying, bishop urge Catholics to speak up
Sherrington replied to Crux about the Bill, saying there are “too many unanswered questions” about the Bill even for supporters of assisted suicide, and it shouldn’t be passed.
The bishop also said the Church supports palliative care for those approaching death, and that is where the government should be improving peoples’ lives in their final stages.
What follows is the full interview with Sherrington.
Crux: During the discussions on the proposal for “assisted death” it looks like the ultimate High Court Judge safeguard will be removed. What is your reaction to this?
Sherrington: I am interested that you use the term ‘assisted death’ which you rightly place in inverted commas. During the present debate, the bishops have used the term ‘assisted suicide’ for very good reasons. ‘Assisted death’ or ‘assisted dying’ are words used by the proponents of this Bill. They are euphemistic and try to obscure the reality of the Bill, which will permit a medic to assist the suicide of a person when they desire it under specific conditions. This is presently prohibited in the law which protects the most vulnerable.
There is an amendment before Parliament which removes the role of the High Court Judge. The amendment talks of review by a psychiatrist, a social worker and a lawyer. How adequately can this review be made? The facts that need to be considered are the medical condition, the freedom from coercion, and compliance with the law. I am fearful that the removal of the so-called safeguard of the High Court Judge further erodes the safety of the Bill. How can we be sure that this “panel of experts” has the knowledge particular to each person who is requesting assisted suicide? Will there be an appeal against a view of the panel? What are the costs of such a policy and how will it be funded? I am fearful that this proposal will divert resources from an already stretched NHS [UK’s National Health Service] and further limit scarce resources for good palliative care.
This panel will not take decisions in the same way as a judge. It is highly likely that the “experts” will favor assisted suicide as a matter of principle so that they can participate. There are too many unanswered questions for a matter as important as this. I therefore stand firm in my belief that the Bill is unsafe and that there is a danger of coercion and control of vulnerable people.
The Assisted Suicide Committee voted against pain being added as a qualifying criteria – for many supporters, this was the chief reason to back the Bill. How would this – being assisted in suicide for depression, anxiety, or even for fearing the financial burden it might place on your family – affect things in Britain?
Regardless of the initial criteria under which assisted suicide is permissible, evidence from other jurisdictions strongly suggests that they will be rapidly loosened. We can think for example of the widened application in Canada and Belgium. In Canada, one in twenty deaths are from assisted suicide.
Your question raises concerns about a number of mental health issues which might lead people to request assisted suicide. The knowledge and treatment of mental health issues has increased rapidly in recent years and we are now more sensitive to the reality of these illnesses. Slowly the stigma associated with them is breaking down. Such challenges call for help in life, treatment and care rather than death. The Bill has promised that freedom will be needed to end one’s life. These mental health issues reduce human freedom and make me more fearful about the danger of coercion of highly vulnerable people. We need to help people live with these illnesses in the best possible way.
You mention the fear of being a financial burden to the family. There are wider questions of how health and social care is funded at the end of life which go far beyond this present debate. These are questions for further political and social debate which not be short-circuited by this particular Bill. Catholic social teaching can help in this future debate.
It is important to distinguish between pain and suffering. Palliative care has led to major advances in the pain control of symptoms. This care needs to be more widely available to people. Experts in palliative care also speak of emotional pain, and spiritual or ‘soul’ pain. These can be relieved by holistic professional and spiritual care. Often listening and allowing a person to tell their story leads to healing and reconciliation with the past. People carry within their hearts and bodies the pain of unresolved conflicts, relationship breakdowns and trauma. Good holistic care can assist a person live with and through these challenges.
Suffering is a complex theme which is part of the human condition. It is idealistic to think of life without suffering. The question of why the innocent suffer has been at the heart of philosophical and theological debate over the centuries. This becomes even more crucial when we deal with assisted suicide because what is proposed here is the termination of human life. If we do that, we deny ourselves the chance to respond to suffering in a truly humane way, in the fullness of freedom and love. Suffering needs to be addressed compassionately in a safe and loving environment. This is the project Dame Cecily Saunders began with the modern hospice movement, inspired by Christian values. A holistic palliative care approach, which incorporates not only the alleviation of physical pain, but also personal accompaniment, spiritual and physical guidance, friendship and care is the right and humane answer to pain.
As a Catholic bishop, I recognize the resources that the Catholic Church brings to sick people; the sacrament of the sick, viaticum, and the importance of prayer for the dying. Catholic chaplains and other chaplains and faith advisors help people in hospitals and hospices and their contribution to the debate cannot be underestimated.
How does the Church deal with people suffering, and with painful deaths? Shouldn’t people avoid it if they are given the opportunity?
The Church continues the mission of Jesus Christ who healed the sick and freed people from the burden of sin. The Lord Jesus healed, performed miracles, and sent His disciples to do the same. This approach to care has been driving the Church’s mission since its foundations and has seen the Church striving to found hospitals and clinics, alleviate suffering in the world and to be close to those who are vulnerable, suffering, and sick. Medicine treats illness and alleviates pain. The Church is the largest non-government provider of healthcare worldwide and Christian hospices in Britain are widely admired.
In her wisdom, in a tradition forged since medical advances in the sixteenth centuries, the Church recognizes there are “limits to treatment,” which we can accept. We do not suggest that people should be kept alive at all costs by what we describe as “extraordinary means.” There comes a point when a person, because of their underlying condition, may refuse further treatment and accept care which respects the dignity of the human person. This is the alleviation of suffering in its true meaning, not its elimination, which is what assisted suicide seeks to obtain. A person may exercise his or her autonomy about treatment but not intend to end their life prematurely and deliberately.
Recently, the press had a lot of news about the use of “buffer zones” around abortion clinics in the UK. Does the move to legalize assisted suicide show a different attitude towards life-and-death in Britain?
There is always a danger in conflating issues but what links these two subjects is the high value placed on personal autonomy and the need to protect personal choice.
While autonomy is an important value, it is only part of the understanding of the human person who has dignity and is relational. It is impossible to assert personal autonomy without first recognizing the unique value and dignity of human life, which begins at conception and ends with natural death. That is why it is wrong that personal autonomy overrides the life of the child in the womb whose dignity is not respected. This approach also fails to recognize the reality that humans are relational beings who live in the world through their relationships with others, with emotions, affections and love. These bond them to other human beings and the whole of creation. Every action of a person touches and affects others, often in unknown ways.
Both these laws overly value personal autonomy and do not consider the wider implications on other human lives. The use of buffer-zones was considered necessary by parliamentarians to protect women who chose to seek an abortion. Women were already protected by laws against harassment and coercion. The presence of others praying or handing out leaflets to offer an alternative was rejected. I fear that the assisted suicide legislation will not adequately protect the right to conscientious objection or freedom from referral to another doctor which further erodes a view which rejects such legislation. While some protection is given for doctors, what about all the other healthcare professionals who work in multidisciplinary teams caring for people at the end of life. They too deserve freedom of conscience.
How would assisted suicide affect the relationship between doctors and patients?
Doctors commit themselves to healing and saving lives. The Greek foundations of medicine led to the Hippocratic Oath which promised to heal and not do harm to a patient. This principle has governed medical practice until the last sixty years when the focus becomes autonomy and choice, especially about the future of the life of the unborn child. Christian healthcare professionals take inspiration from the life of Jesus Christ who healed the sick.
Good communication between the patient and the doctor requires the building of trust. In fact, recent cases of medical mismanagement and doing harm show the vulnerability of the patient who entrusts himself or herself to the professionalism of the physician. Language challenges, and the pressure under which the health service operates, can weaken the relationship which is needed between the doctor and the patient. The danger of this Bill is that people may be anxious about whether the doctor really cares for their healing and whether they can trust the physician.
This radical change in law, which crosses a watershed, will fundamentally alter the relationship between doctors and patients which could, in turn, have a detrimental impact on the whole of healthcare provision. This might cause some people to fear using healthcare – especially the elderly and vulnerable. The possibility for doctors to suggest assisted suicide as well as the duty of referral, which infringes the right to conscientiously object, would put a strain even on the relationship between doctors who oppose assisted suicide, and their patients. Instead, patients deserve access to safe healthcare, and doctors who are able to perform their role as caregivers and guardians of human dignity.
Thank you for the opportunity to answer these questions, As a final point, it is the duty of every MP to ensure that any proposed change in legislation has sufficient time for debate and full examination of its implications. I do not consider that this Bill has had sufficient time for debate and scrutiny, as it has been a Private Members’ Bill, and so I believe it should be rejected outright.
Follow Charles Collins on X: @CharlesinRome