LEICESTER, United Kingdom – Euthanasia is a violation of millennia-old medical ethics, and a patient seeking death from a doctor is antithetical to what it means to be a physician, says a leading American medical ethicist.
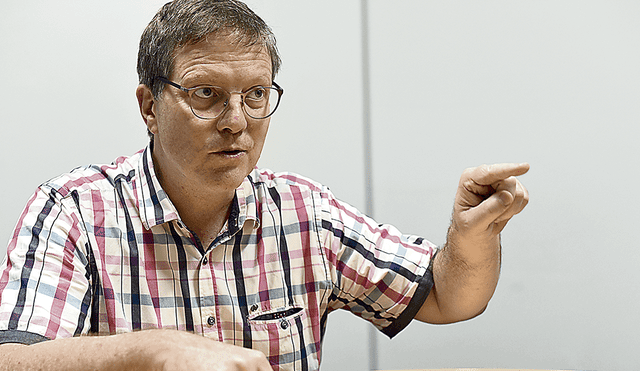
Dr. Mark Komrad – a clinical psychiatrist and an ethicist who is on the teaching Faculty of Psychiatry at Johns Hopkins, Sheppard Pratt, and the University of Maryland – told Crux this is even more true for psychiatric patients.
“It is an anathema, it is an inversion to put psychiatrists particularly, of all specialists, in the position of diverting their patients towards death,” he said on the sidelines of a half-day symposium on the ethics surrounding suicide and euthanasia which took place July 7 at the Oxford-based Anscombe Bioethics Centre, the leading Catholic institute in the field in the United Kingdom.
Komrad said this goes back further than the origins of Christianity and notes the Hippocratic Oath in ancient Greece forbade killing patients even if asked by them, and this is what distinguished it from other schools of the era.
“The general principles of medical ethics – the fundamental ethos of medicine – was to not administer death. Rather it was to provide comfort, to sometimes get out of the way of death, but certainly not in any systematic and groupthink or legal way, to administer death,” he said.
Komrad was a key influence on the statement by the American Psychiatric Association on medical euthanasia, which states “that a psychiatrist should not prescribe or administer any intervention to a non-terminally ill person for the purpose of causing death.”
RELATED: Belgian ethicist says euthanasia has become ‘sacralized’
“We have a skillset that can help people find somehow a path to a better future or to try at least to do our best to mitigate suffering, to provide hope, to travel with patients in their suffering,” he told Crux.
“So we can do all of those things, but we prevent suicides, we do not provide suicides. That is our message when working with individuals, and it is also very much our public message when it comes to public health and our campaigns in society to try and mitigate suicide and steer people towards treatment,” Komrad said.
The psychiatrist – who is Jewish, not Catholic – said a “post-Catholic” ideology is at play in traditionally Catholic countries such as Belgium to legalize euthanasia for non-terminal patients.
“There is a powerful rising tide of secularism in general in Belgium, and specifically a rejection of its long historical Catholic character and roots … So, this idea of Belgium trying to redefine itself, reestablish its identity as a sort of post-Catholic, secularist culture, is a critical counterpoint to the fundamental objection to euthanasia that arises out of a set of Catholic values, increasingly considered obsolete by many in Belgium. Those same values had been promoted to object to abortion,” Komrad said.
He spoke to Crux about euthanasia and psychiatry, the post-Catholic ethics in Belgium, and how society should view medically-assisted suicide. Here are excerpts of that conversation:
Crux: You have called euthanasia for mental health patients an “inversion of psychiatry’s fundamental values.” What do you mean?
Komrad: We in medicine have a venerable tradition of ethics of our own. We have developed it in a thoughtful, even scholarly fashion, as well as by its actual practitioners and by professional societies. There has also been much medical-ethics scholarship in a tradition that is actually longer than other venerable traditions, such as the tradition of the Church and Christianity. We actually go back an additional 300 years before the beginning of the Church. We have our origins in a very specific set of values, in the Hippocratic origins of medicine.
The cult of Asclepius [Greek god of medicine – ed.] was ramified into a variety of different cults in ancient times, and one of them was the school of Hippocrates. In order to be part of the school for training and for treatment, one had to profess a set of values (the origin of the word profession). In fact, one had to take a specific oath, an oath that actually became core and almost definitional to the acculturation and entry into the medical profession for the next 2,500 years: The Hippocratic Oath.
One of the things that distinguished the cult of Hippocrates from the other Asclepian cults was that they would not perform euthanasia. In the oath, there is one particular phrase: “I will give no man a poison, nor advise anyone else to do so.” That was actually one of the distinguishing characteristics of Hippocratic Medicine. It was out of those roots that the mighty tree of Medicine grew for the next two millennia, much like the mighty tree of Christianity and the Church grew out of the cult of Jesus Christ, one of a number of other messianic cults at the time, which professed some specific and powerful values that ended up suffusing the tree of Christianity, as it grew into a mighty oak, much like the tree of Medicine.
So an original and enduring principle of medical ethics – the fundamental ethos of medicine – was to not administer death; to provide comfort, to sometimes get out of the way of death, but certainly not in any systematic and groupthink way, legal way, to administer death. Now within that medical ethos arises psychiatry: Psychiatry is the specialty that ministers to the mind, to the suffering heart, to the suffering brain, and, as a matter of fact to the suffering soul.
In doing so, what psychiatry has cultivated is an ethos that tries to help people in the midst of that suffering, with their despair, with their demoralization, with their hopelessness and helplessness. These goals are independent, by the way, of any specific ‘diagnosis.’ Psychiatrists, of all physicians, have a particularly developed skillset that can help people find somehow a path to a better future, or to try at least to do our best to mitigate suffering, to provide hope, to travel with patients in their suffering. The word compassion means ‘to suffer with.’ So we take a compassionate journey with them, to try and address some of the various psychosocial forces that may be part of that suffering, to continue to administer, when available, other kinds of treatment for that suffering.
Indeed, psychiatrists and other mental health professionals even have a capacity to help people make meaning of suffering, and this is certainly something with which the Catholic Church would be familiar. This is one way in which the psychiatric profession and the Church are quite congruent. So we can do all of those things, but we prevent suicides; we do not provide suicides. That is our message when working with individuals, and it is also very much our public message when it comes to public health and our campaigns in society to try and mitigate suicide and steer people towards treatment. It is an anathema, it is an inversion, to put psychiatrists particularly, of all specialists, in the position of diverting their patients towards death. Not only that, it provides a tempting and seductive shortcut for exhausted treaters, exhausted families, exhausted patients, and exhausted insurance companies and funders, to be able to divert the attention, energy, devotion, resources, and advocacy from opening the otherwise stenotic channels of access to mental health care.
I had a patient who had liver failure. This was patient with a chronic mental illness that I really wanted to get into a very expensive treatment option that I have found has been remarkable at turning many patients around – a very high end long-term residential treatment. The third-party insurance carriers would not pay for that. However, they paid for a liver transplant which failed, and so they paid for a second liver transplant at the total cost of over $2 million. Yet they would not pay for what I felt would be a powerfully ameliorative psychiatric treatment that would turn around his chronic mental illness, at a fraction of that cost.
In a society where there is euthanasia for such a patient, the patient, the family, the insurer, and the physician all turn their attention away from that kind of advocacy into the short circuit of death, through euthanasia.
When you went to Belgium, you said that the country’s Catholic religious background plays a role in its acceptance of euthanasia. What do you mean?
That actually emerged out of a fascinating discussion that I had with Didier Pollefeyt, Professor of Theology and Religious Studies at the University of Leuven – the big Catholic university there. He tried to help me understand that to really appreciate where a lot of the energy is coming from in the Belgium story, I had to understand the post-Catholic culture of Belgium.
He explained to me that there is a powerful rising tide of secularism in general in Belgium, and specifically a rejection of its long historical Catholic character and roots. So, this idea of Belgium trying to redefine itself, reestablish its identity as a sort of post-Catholic, secularist culture, is a critical counterpoint to the fundamental objection to euthanasia that arises out of a set of Catholic values, increasingly considered obsolete by many people in Belgium. Those same values had been promoted to object to abortion. So, it is just an old wine in a new flask, say the secularists.
So, as far as the secularists are concerned, it is the same tired arguments that do not stand up to the modernist, liberal apotheosis of autonomy and self-determination, which elevates those values so that they trump all other values – especially the dignity and preciousness of life. Any attempt to resort to that argument about the preciousness of life, in Belgium, apparently gets one accused of being a Catholic, a crypto-Catholic, or unduly influenced by the residuum of the Catholic legacy. It becomes sort of an ad hominem argument against those who would object to euthanasia. Objectors are not getting with the program of this ‘moral pioneering’ that the secularists feel they are accomplishing in Belgium to promote people’s autonomy and self-determination – a showcase of those values to the world. Belgium is no longer, as perhaps it was in centuries past, a showcase of Catholicism.
Do you think this will keep families from seeking help for their loved ones with mental health problems, if they think euthanasia will be an option?
I certainly think that knowing that physicians can administer death as a treatment plan disrupts the fundamental trust people have in physicians. As a matter of fact, it is something that has been in the conversation for several millennia: that there is sensitive trust that comes in a treatment relationship where you arrive so vulnerable.
The power of medicine is suggested by the Asclepian symbol, the snake. It can have healing powers or poison powers. The physician will wield the art and science of Medicine with tremendous caution, so that you are in the hands of somebody who could, but will try not to hurt you.
If you look at some of the more recent polls, you see strong support for euthanasia laws. As a psychiatrist, what would you tell the general population about euthanasia?
Most people do not understand, because they do not need to understand, the state of the art of palliative care. There is so much that contemporary palliative medicine can do to help. The capability to minimize symptoms, minimize suffering and allow people to maintain a fair amount of dignity is highly developed within the state-of-the-art of palliative care. Euthanasia is a big challenge to clinicians in palliative care, and many of them are despairing that they are being misunderstood and underutilized.
The other thing is, I think people need more education about what it means to be a physician. That is something that is often left out of this conversation in the public domain; what it’s like on the doctor’s side. It as if the doctor’s feelings, rights, ethics, and experience are irrelevant. We are in a highly consumerist culture in which the doctor is increasingly seen as the servant of society. If the patient comes and asks you to jump, they expect the doctor to simply respond, “How high?”
I think one of the things the public needs to understand is the culture of values that we acquire in the course of becoming a physician. Euthanasia is antithetical to what it means to be a physician, especially what it means to be a psychiatrist. In fact, consider a patient who comes knocking on the door of a doctor, particularly a psychiatrist, and says, “Doctor, I am coming and laying before you a request, to kill me.” I actually think that’s an ethical violation on the part of the patient: to put their doctor in that position to have to consider that request, to assume that would be in our purview of ethical practice. This a terrible position in which to put a physician, even where it’s legal. It is an anathema to medical practice, and especially to a psychiatrist, to be asked by a suicidal patient to provide them the suicide they are desiring.
“Of course there are always a few doctors that are somehow inured. You see this in Oregon, Washington, Belgium, and the Netherlands. A small handful end up being the ones who provide the majority of assisted suicides and euthanasias. There is one psychiatrist, Dr. Lieve Thienpont in Belgium who does about 60 to 70 percent of all the psychiatric euthanasia. She has developed her own sort of immunity to it, In the Netherlands, there is a culture within the the Levenseindeklinieks which provides euthanasia. Those who are working in those clinics have really bought into a groupthink that they are engaged in a great virtuous labor. But the fact of the matter is that for the majority of physicians this is profoundly painful.
In Canada, we are seeing the emergence of a building wave of physician conscientious objectors, against providing euthanasia. The Canadian government, especially in Ontario, is now beginning to have legal proscriptions against conscientious objection, so that it is starting to become illegal to even refuse to be part of the referral machinery. That doesn’t mean you have to do it yourself, but what it does mean is that you will be accused of abandoning your patient if your he requests euthanasia and you don’t help the him find a practitioner who is possibly willing to do it, if you personally object to it. I call this Euthanasia – Phase 2.0: shutting down conscientious objection.
I am very interested in other historical examples where the medical profession, and psychiatry in particular, lost its ethical moorings because of powerful changes in social mores that swept physicians up in the torrent of radically changing values. Specifically, I have started to lecture widely about two linked historic epochs: the eugenics and sterilization movement in the United States and the Nazi T4 program to exterminate the mentally ill.
In both of these cases, these were engineered and deployed not by rogue psychiatrists and bad apples; these were the leading figures of their times: the heads of departments, chairmen, mentors, celebrated professors, and presidents of the German psychiatric associations that concocted and implemented these horrendous programs. Now, in historical retrospect, we look back and we say, “My God, what were we thinking?” At the time, they too felt that they were moral pioneers and that they were engaged in a great and virtuous revolution of morality.
So, history teaches that physicians can be very vulnerable to becoming fish that are swimming in the same toxic water as the societies in which they live, and not realize it at the time. I think this is what is happening now in Belgium and the Netherlands with doctors and their medical associations. It was not until 2010 that the German Psychiatric Association apologized formally for its prominent role in the Holocaust, acknowledging, “what were we thinking back then!?”
[This article has been edited since publication to clarify sections of the transcript.]