VATICAN CITY – The Vatican has issued an updated version of their charter for healthcare workers, removing question marks from modern ethical concerns such as euthanasia and the creation of human-animal chimeras by offering a clear set of guidelines.
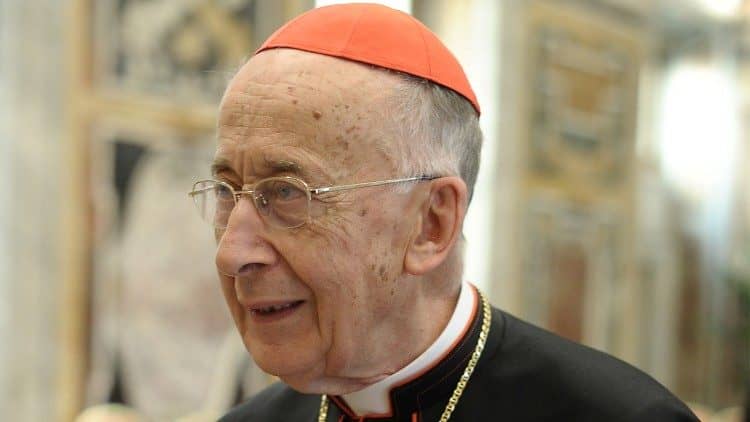
In the past 20 years “there have been two situations, two events” that have made the production of a new healthcare charter necessary, Professor Antonio Gioacchino Spagnolo told CNA Feb. 6.
The first, he said, is “scientific progress. In these 20 years there has been a lot of scientific progress in the field of the beginning of life as well as in the phase of the end of life, in the context of living.”
But alongside advancements in science the Church’s Magisterium has also produced several texts dealing with new and current issues, offering an authoritative take on how they should be handled.
The charter, he said, “encompasses a sort of collection of the various positions there have been, the various pronouncements, keeping the progress of bio-medicine in mind.”
Spagnolo, director of the Institute of Bioethics and Medical Humanities at the Faculty of Medicine and Surgery at the Catholic University of the Sacred Heart in Rome, spoke to journalists at the Feb. 6 presentation of the new charter, and played a key role in drafting the new text.
A first edition of the charter was published in 1994, but in the wake of broad scientific advancements and various updates in the Church’s Magisterium, the Holy See Monday rolled out the new version of the charter for healthcare workers.
Released to coincide with the annual World Day of the Sick celebrations taking place in Lourdes, the updated charter includes all magisterial documents published since 1994 and will be sent to bishops’ conferences around the world.
At roughly 150 pages including the index, the charter is structured much like the old edition, and is divided into three parts: Procreation, Life, and Death.
The section on procreation covers everything from contraception, IVF, and the scientific use of embryos, including freezing them, as well as newer topics such as the mixing of human and animal gametes, the gestation of human embryos in animal or artificial wombs, cloning, asexual reproduction, and parthenogenesis.
In the “Life” section, topics covered are “all of the health events that are in some way connected to living,” Spagnolo said, including vaccinations, preventative care, drug testing, transplants, abortion, anencephalic fetuses, as well as gene therapy and regenerative medicine.
The social part of the charter also covers areas specifically linked to poverty, such as access to medicines and the availability of new technologies in developing countries or countries that are politically and economically unstable. Rare and “neglected” diseases are also covered in the new text.
In his comments to CNA, Spagnolo commented on recent cases the new, updated charter would cover, including the creation of human-pig “chimeras,” as well as the case of an elderly woman with dementia who was held down by her family during a euthanasia procedure.
The first case refers to the recent high-level scientific research project that culminated in the creation of chimeras, or organisms made from two different species.
While the project initially began by conducting the experiment on rats and mice, at the end of January it culminated with the human-pig mix, marking the first time a case had been reported in which human stem cells had begun to grow inside another species.
In the experiment, which appeared in the scientific journal “Cell,” researchers from various institutes, including Stanford and the Salk Institute in California, injected pig embryos with human stem cells when there were just a few days old and monitored their development for 28 days to see if more human cells would be generated.
Human cells inside a number of the embryos had begun to develop into specialized tissue precursors, however, the success rate of the human cells overall was low, with the majority failing to produce human cells.
Commenting on the case, Spagnolo said this type of “hybridization between human and animal cells” was primarily done to garner more scientific information. “It’s important” that this research is done, he said, but cautioned that we can’t be “indifferent” to how the information is used.
If a scientist decides to mingle human cells with those of another species in order to create some sort of hybrid being, “this is of course something that can’t be accepted because in some way it means using the generation of a life as an instrument to reach one’s own ends.”
However, if it’s done for a purpose other than generating alternate beings, such as growing human organs for transplant, Spagnolo said this would be acceptable.
One thing that’s already being proposed, he said, is the possibility of xenografts, i.e. tissue grafts or organ transplants from a donor that is a different species than the recipient.
The idea of doing this, Spagnolo said, is to “inoculate” pigs with human cells, allowing the organs of the pig to receive human antigens, “so when a transplant is done with a liver or heart from the pig inside a (human being), there wouldn’t be the rejection that there is normally doing it with other species.”
Spagnolo said that using the hybrid cells for organ or tissue transplant “is acceptable because to transfer a human cell to a pig doesn’t mean creating a life.”
Rather, it allows the pig “to have a genetic patrimony similar to that of a human being to then be able to use the organs to help people,” he said, emphasizing the fact that it’s not pig cells being injected into human beings, but vice versa.
So to make a good, informed decision involves first of all seeing “what type of experiments” are being done, deciding from that “whether it’s acceptable or not,” then looking at what “one intends to produce, what are the objectives one intends to reach.”
Pointing to another touchy scientific case that came up recently when an elderly woman in her 80s was held down by her relatives as her doctors euthanized her, Spagnolo said this is the type of murky water which “advanced statements” or living wills wade into in countries where euthanasia and assisted suicide are legal.
The woman, who lived in the Netherlands, had dementia and had reportedly expressed a desire for euthanasia when “the time was right” at an earlier date, but had not done so recently.
When the woman began exhibiting “fear and anger” and was sometimes found to be wandering the halls of her nursing home, the senior doctor at the home determined that the woman’s condition meant the time was right, and put a sleep-inducing drug into her coffee so he could administer the lethal injection.
The woman was not consulted, and woke up as the doctor was trying to give the injection. When she fought the procedure, her family members were asked to hold her down while the injection was completed.
“When medicine no longer does what it should” because in a living will someone expresses their desire for assisted suicide, “this statement completely alters the doctor-patient relationship,” Spagnolo said.
He pointed to a bill that is currently on the table in Italy that would effectively legalize euthanasia and assisted suicide, requiring doctors to act on the advanced statements of their patients in this regard, and prohibiting them from conscientious objection.
This bill, as well as the case of the woman in the Netherlands, illustrates “the difficulty of advance statements,” Spagnolo said, explaining that if someone makes an advance statement and later decides against it, “the fact of having said it before is used and is done (by) drugging the patient.”
While the doctor-patient relationship is always a key element of the discussion, Spagnolo noted that various studies have been conducted showing a doctor’s behavior toward patients differs based on whether or not the patient has an advanced statement, specifically on euthanasia.
“This disparity should be avoided. The doctor should always act the same way when the person is concerned,” he said.
So with the new charter, all healthcare workers will now have a point of reference for some of these sticky scenarios, he said.
“They can know that some things must be done, they are obligatory. Others, however, are only possibilities.
In this sense, “the will of the patient is very important, not in the perspective of ‘anticipating’ death, but in the perspective of knowing whether or not to accept and support certain interventions the doctor can do, but which the patient might think unsuitable.”