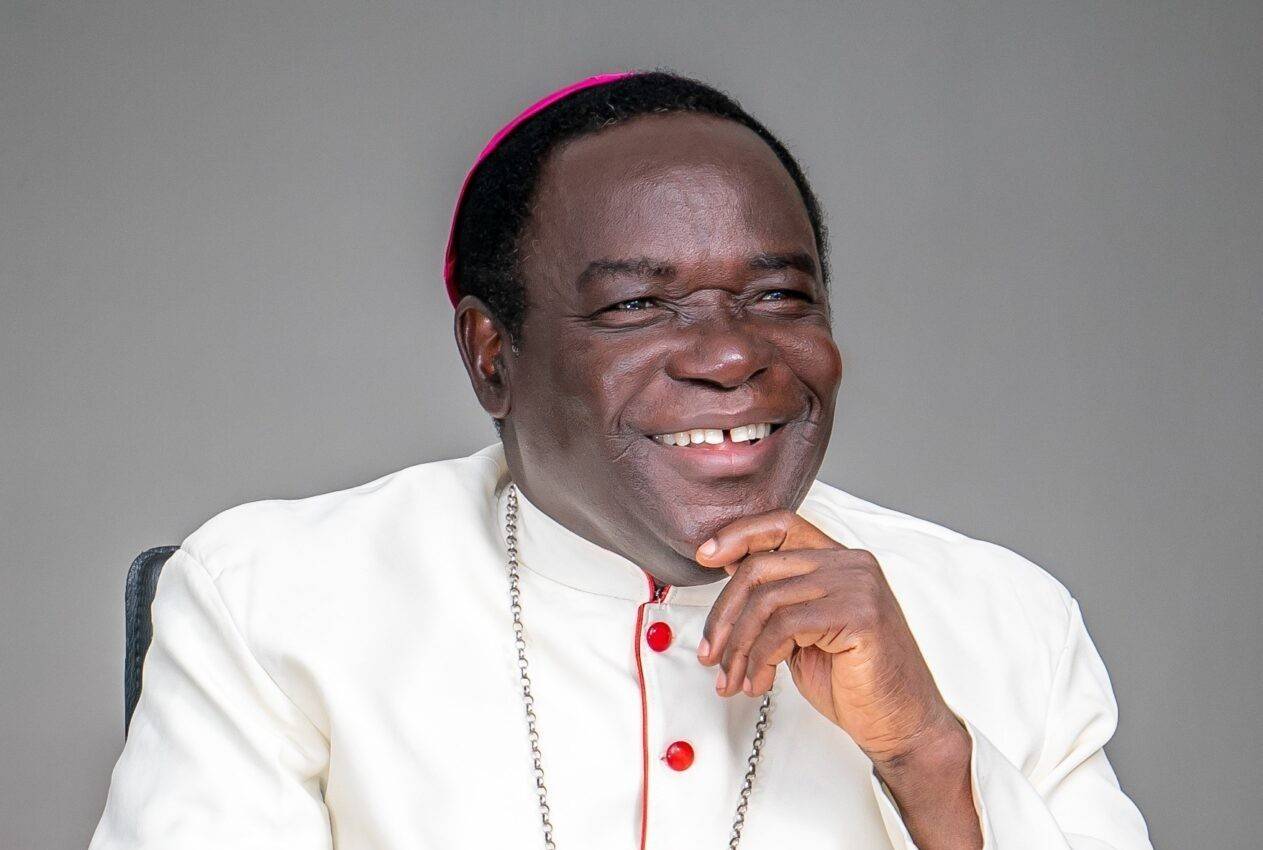
CAPE TOWN, South Africa — Churches need to make it their mission to get people in developing countries vaccinated against COVID-19, said a representative of the Symposium of Episcopal Conferences of Africa and Madagascar.
This is “a matter of life and death,” Bishop Sithembele Sipuka of Umtata, South Africa, second vice president of the symposium, SECAM, told Catholic News Service. The vaccine “is not a luxury, it should be a common good,” he said.
Churches throughout the region, including South Africa, are using parish structures to “address vaccine hesitancy and dispel myths,” said Sipuka, who is also president of the Southern African Catholic Bishops’ Conference.
Africa has recorded more than 8.3 million COVID-19 cases, yet it suffers a severe shortage of vaccines, said Project HOPE, a U.S.-based nongovernmental organization that works with health ministries in other countries. Noting that “it is well understood that as long as the virus spreads and mutates in some parts of the world, no place will be safe,” the project said that “out of 5.7 billion doses of coronavirus vaccines administered around the world so far, only 2% have been in Africa.”
Catholic Relief Services said it is “unacceptable that only 15% of the promised vaccine donations from wealthier nations have materialized in low-income countries.”
“Vaccine hesitancy, disinformation and access are among our top concerns in the 110 countries where we work,” the U.S. bishops’ international relief and development agency said. “We’re also extremely concerned that local health systems in low-income countries cannot handle such large vaccine rollouts without significant additional support.”
The church is doing what it can to help in African countries that do not have the necessary facilities for large-scale vaccination, Sipuka said.
“A big advantage of COVID-19 vaccination is that it is simple to do,” compared with treating people infected with HIV, he said.
“You just need to have one or two jabs in the arm and you are safe. And you can have this as long as you are not ill,” the bishop said. Treatment for the virus that causes AIDS must be taken regularly and requires adequate nutrition to be effective, he said.
With government-mandated lockdowns, which prevented people from attending Mass and other church activities, the church’s “ability to making a meaningful contribution was curtailed,” he said. But now that restrictions have been largely lifted, “the church has more access to people to motivate them.”
“We must support each other in embracing life by vaccinating,” Sipuka said, noting that “these conversations need to happen.”
In Liberia, as soon as vaccines become available, people line up to get them, Abena Amedormey of CRS said from the capital, Monrovia.
In Monrovia, “the first question people ask each other is ‘Are you vaccinated?’ and the answer is ‘Yes,'” she said. But in other parts of the country of 5 million people, vaccination teams are waiting for supplies to take to remote areas.
A CRS survey early this year found a “large level of trust in the World Health Organization and the government,” Amedormey said, noting that, across West Africa, there is a history of dealing with pandemics. “Protocols like wearing masks, hand washing, social distancing are familiar,” she said.
A 2014-2016 Ebola epidemic in West Africa, including Liberia, killed more than 11,300 people.
Noting that Liberia does not have the infrastructure to store vast quantities of vaccines, Amedormey said equipment and training to manage vaccination are needed along with doses.
“Health workers who are trusted in communities are part of the COVID-19 vaccination teams” that CRS and others have helped train, she said.
In Madagascar, where only 1.5% of the population of 27.7 million have been vaccinated against COVID-19, the health care system is very weak, and people are reluctant to be vaccinated, said Tanja Englberger of CRS.
The East African country, which is part of the vaccine-sharing mechanism COVAX, has received just over 1 million vaccine doses since May, “much later than other countries,” she said.
For Catholic Relief Service’s 650 staff, mostly field workers, there was much “anxiety knowing the rest of the world was being vaccinated,” Englberger said in an Oct. 4 interview from the capital, Antananarivo. She said there were many infections among staff and deaths of family members during the island’s second wave in April.
But many Malagasy “don’t trust the vaccine,” Englberger said, noting that people told CRS that they “don’t feel it’s necessary or are afraid of its side effects.”
A lack of reliable information about the vaccine and its availability is among the reasons people are reluctant to be vaccinated, she said.
“The amount of effort it takes to persuade people who rely on herbal remedies (to be vaccinated against COVID-19) is incredible, even people who have plenty of information” about the vaccines, she said.
Weak road structures and rocky terrain are also barriers to getting people vaccinated on the island, which is 227,000 square miles, Englberger said. “People often don’t realize how big Madagascar is,” she said.
The World Food Program warned in May that 1.14 million people in the south of Madagascar face high levels of acute food insecurity and, of these, 14,000 were in the catastrophe category.
In places where there is conflict and instability, such as South Sudan and northern Mozambique, “it’s very difficult to get people vaccinated” against COVID-19 because facilities cannot function if it is unsafe, Sipuka said.
Bishop Macram Max Gassis, retired bishop of El Obeid, Sudan, said early this year that the malnourished people in Sudan’s Nuba Mountains are “moving skeletons,” and their compromised immune systems expose them “to all kinds of diseases, not just COVID-19.”
“As church, we don’t have the capacity to get involved in vaccination. We are overwhelmed feeding the hungry” in South Sudan and the Nuba Mountains, Gassis said.
In May, South Sudan returned 72,000 of its 132,000 vaccine doses to the COVAX facility for use in other countries before the doses expired. Its health ministry said the doses were unused because of delays in approving the vaccine’s use, slow training of vaccinators and slow initial vaccine uptake by health care workers, Voice of America reported.