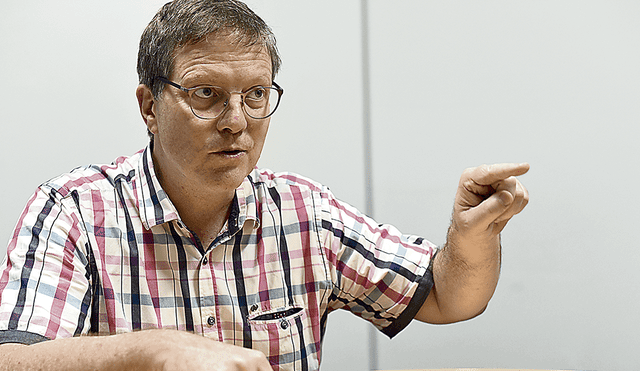
[Landon Roussel is a pioneer in direct primary care, where doctors directly bill their patients without the intermediary of insurance companies, and the owner and chief medical officer of Communitas Primary Care. While an undergraduate at Rice, he spearheaded donation drives and multiple medical mission trips to Mexico and Guatemala. In 2010, he was a member of the inaugural medical cohort for Fellowships at Auschwitz for the Study of Professional Ethics (FASPE) through the Museum of Jewish Heritage. Most recently, he has advocated to congressmen and senators for more transparent pricing for patients in Washington, D.C and Louisiana. Roussel produces and hosts ‘The Direct Primary Care’ podcast and is also author of the book, On the Primitive Way, a religious travel memoir. He spoke to Charles Camosy about incorporating his faith with his medical vocation.]
Camosy: Tell us about how you got into medicine. What drove you into the field? Where did you end up studying?
Roussel: I was inspired to go into medicine after going to the memorial service for my maternal grandfather. I always thought I was going to be an engineer like my father. My grandfather and nearly all of my uncles worked at the plants and that was the only family I got to know as a child — I spent very little time with my mom’s family. I made good grades in math and science and thought, naturally, I would follow in my dad’s footsteps. When I went to his funeral however, I got to know who he was — an artist, a journalist, a lover of nature, and, most importantly, always eager to experience the human condition each day. When I hear his friends talk about who he was, I saw that in myself, a desire to get to know people each day, experience life with them in their sufferings and in their joys and to use my talents to help them. After the funeral I decided I would enter medicine.
That was when I was fifteen, and ever since then I’ve worked hard in my studies to have the skills needed to be that doctor who could help people when they are going through tough times. This drive led me to pursue the best opportunity available to me to become a good doctor. I ended up getting my medical degree at Weill Cornell Medical College in New York City and then completing a residency in internal medicine with primary care focus at Harvard Medical School/Mt Auburn Hospital.
I got to know you, and your strong Catholic faith – I recently discovered that you are a fourth degree Knight of Columbus – when you took my bioethics graduate course while studying at Cornell. Did your Catholic faith drive your interest in bioethics? How was it being a person of deep faith at a school like Cornell?
Absolutely.
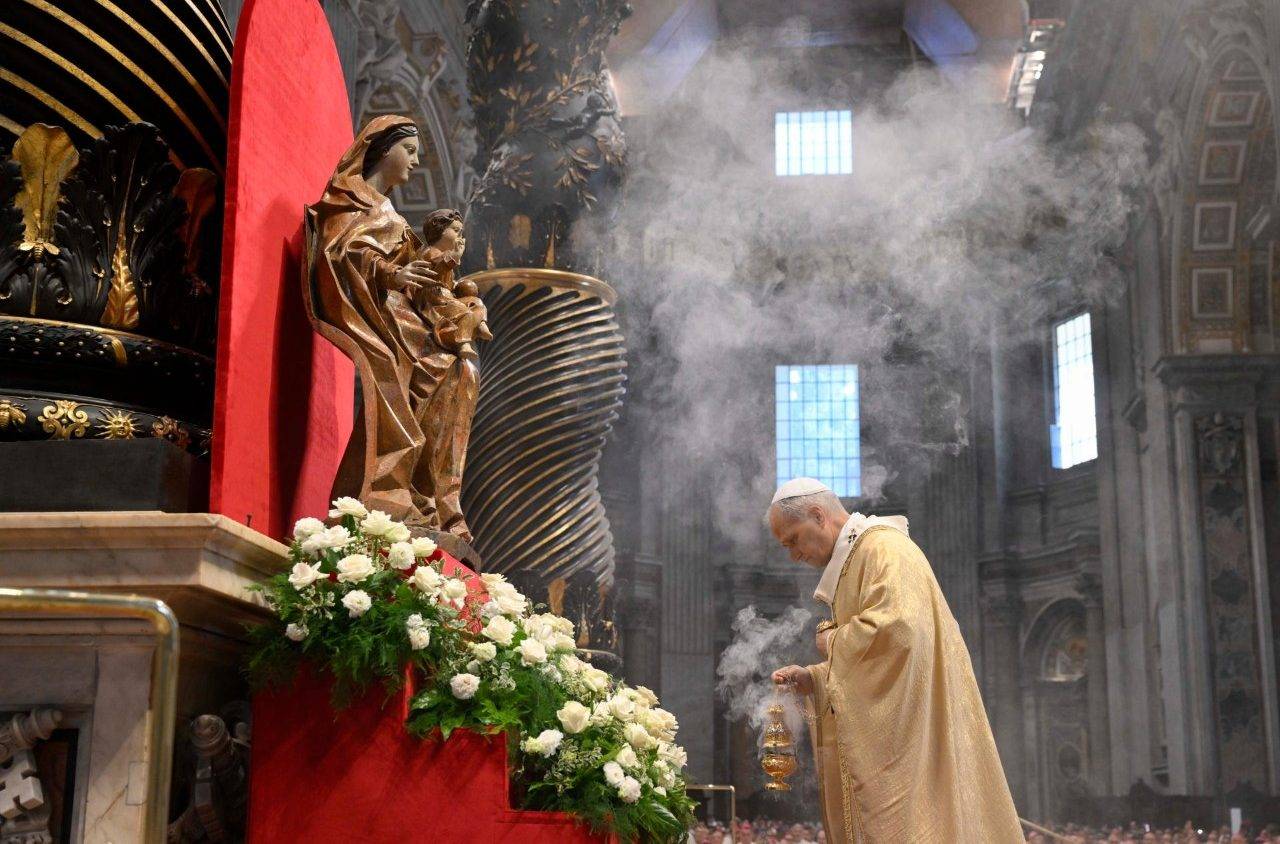
As a Catholic convert, my faith has always been central to my work as a doctor. I grew up as a generic Evangelical Christian, but when I went to college, as a young biochemistry major, I contemplated leaving my faith behind, as my upbringing left me with a very paltry defense against secular professors who heralded the wonders of science and the Enlightenment. Yet neither of these offered a persuasive response as to how we should live our lives. This led me to a soul-searching quest that led me home, to the Catholic Church. I was confirmed on Easter Vigil of 2007 along with Amanda, who eventually became my wife. As a Catholic convert, faith became central to my intellectual development, as faith added the fulfillment of reason that shows us how to use our scientific abilities.

What struck me during my training, however, was how devoid medical education was of moral grounding. In healthcare we make moral decisions every day, yet throughout medical school I repeatedly experienced minimization or thinning out of moral learning at the expense of technical expertise. Habermas characterizes the environment well –’Wissenschaftkeit’ — scientificism. Everything that appears technical or scientific takes priority of the questions of morality, values and conscience. This is a very dangerous state for healthcare where we have potential to intervene so dramatically–for good or for evil–in people’s lives.
As a person of faith at a secular medical school, it was at times challenging to defend my faith. I recall my bioethics professor scolding me once in front of the class to “leave scholasticism at home.” That said, I strived earnestly to remain professional and most importantly to defend my positions with cogency and intellectual rigor. My peers respected me for this, even if they disagreed with me.
Then it appears that you got bit by the bioethics bug?
I wouldn’t call it exactly a bug. As a doctor, when someone tells me a bug, it sounds like a temporary virus that comes and goes.
My training in bioethics was not something that came and went but became part of the very fiber of my vocation. What started out as a genuine concern with the moral uprootedness of my profession led me on a path to deepen my own intellectual understanding of the moral basis of healthcare. This started out with your course. The course was so inspiring I knew I needed more. I then went to conferences, published articles and went to every opportunity I could in medical school to deepen my intellectual development in bioethics.
After my third year of medical school, I took a year off to get a Master’s in Bioethics, and after that I continued to present at bioethics conferences and from 2015-2017 participated in the Paul Ramsey fellowship with the Center for Bioethics and Culture. Now I’m slated to teach bioethics at Franciscan University next semester.
How did your medical and bioethics training get you interested in direct primary care?
Just to take a step back, direct primary care is nothing more than being a regular primary care doctor without taking health insurance. Sounds shocking these days but before the 1980s, not taking insurance was virtually the norm. Today we do it by a low-cost monthly fee, though there are certainly some who just charge on a per visit basis.
In any case, my background in bioethics has everything to do with my interest in direct primary care. In keeping with the perennial values of my profession, I wanted to be a doctor who has a long-lasting, deep and abiding relationship with my patients with minimal interference from outside influence. Yet what I witnessed repeatedly throughout my training is outside influence in the doctor-patient relationship, by insurance companies, administrators and government. Direct Primary Care allowed me to take back my profession by minimizing unnecessary involvement of third parties in the exam room.
More than that, however, in terms of economic values, direct primary care is more in line with our Catholic understanding of right ordering of society. In keeping with our understanding of solidarity, provision of social goods should be provided at the lowest level possible.
Healthcare is certainly a social good, and only when its provision can’t be taken care of at a lower level should it be handled by a larger body. Now there’s certainly the case to be made that health insurance can and should be handled by larger bodies — there’s power in numbers. But going to the doctor’s office is not health insurance, and most people can afford to pay for their primary care doctor out of their own pocket.
Your interest in direct primary care was so strong you even went home and opened up a Direct Primary Care practice. How is the practice going? Now that you are in the trenches, what have you found to be the strengths and challenges of the Direct Primary Care approach?
The practice is going well.
I have offices in Baton Rouge, Gonzales and St James Parish. My panel is nearly full, and I love the opportunity to be a full-fledged primary care doctor with the freedom to care for my patients how they need without being told what to do by insurance companies or administrators.
Moreover, we have developed several patient-care niches that are underserved to whom we are offering a genuine value through our services: small-business owners, underinsured patients, home-bound senior citizens and immigrants. These groups often find themselves without health insurance and without access to healthcare, and our approach allows us to provide them quality healthcare, affordably.
Being in the trenches, one of the biggest challenges I’ve faced is dealing with the health insurance mentality. We’ve gotten so accustomed to health insurance paying for everything in our system that it’s become an addiction and it’s colored nearly all of our healthcare choices.
Many people I talk to have gotten used to the view of a primary care doctor as a professional paper pusher and box checker. This is, sadly, what’s become of primary care under the insurance model, a cog in the medical-industrial complex. For thousands of years, however, being a doctor has been about being in people’s homes, being in a solo office and spending time with people, forming relationships. Being a primary care doctor is so much richer and fulfilling than what it’s become under the insurance model. We need to recover the profession, take it back and form it into what it should be. But it takes re-envisioning the way healthcare is done.
My motto for doing this comes straight from the Tantum Ergo–’Et antiqum documentum, novo cedat ritui,’ –’Ancient forms of grace departing, newer rites of grace prevail.’ We need to take what is good from medicine in the past — the relationship, the common sense, the continuity–and throw away what is simply baggage of history — paternalism, closed-mindedness, even greed. This can be done but it takes close discernment of what was good from the generation of doctors who our parents and grandparents used to see and what wasn’t so good that we need to leave behind.